.
Within the suite there is a consulting room, a procedure room and audiology
room with a sound proof booth. Prof conducts clinics at least four times per
week. As the fellow I sat in with Prof and gained valuable insights into the
assessment of the complex otology patient. Prof trained me to undertake
transtympanic ECOG recordings in the procedure room. This is a useful skill to
learn, and I took over this duty during the majority of the clinics. I also
learnt how to perform transtympanic promontory stimulation and performed many
such tests during the fellowship. I am now trying to develop a facility for
transtympanic ECOG testing at my NHS unit.
Prof has
built up a very large Meniere’s practice which allowed me to gain experience
in the management of difficult scenarios such as bilateral disease and the
treatment of resistance cases. For instance I became confident in the use of
transtympanic gentamicin for vertigo control. By having a large cohort of
Meniere’s patients it is also possible to follow the long term course of
disease. This experience as made me very conservative in the use of
destructive techniques, as it is clear that many patients develop bilateral
disease as they grow older.
The
promontory stimulation test has fallen out of favour in many
UK
units, and I rarely performed it in
Nottingham
. In
Sydney
all adult patients receive the test as part of their initial work up for
candidacy evaluation. I soon realised the usefulness of the test. Many adult
patients have not heard anything for some years and the sense of wonder they
feel when they hear a crude electrical sound is amazing. I am sure that this
experience motivates them and their relatives through the following months as
they progress through assessment, surgery and mapping. It also provides great
assistance in determining the side to implant.
The rooms
are run by Cathy and Rosemary under the supervision of Alex Gibson. Together
they provide a vibrant working environment and they are also a very useful
source of local knowledge. By the end of the fellowship I felt a valued and
integral part of the team.
The
Princess Alexandra Children’s Hospital at Westmead
This
hospital is situated in the western suburbs of
Sydney
. It is a new hospital which provides the most comprehensive paediatric
service in
New South Wales
. It has been beautifully
designed with the needs of children and their parents paramount. As such it
was a pleasure and privilege to be on the staff here.
Prof uses
this hospital for electrophysiological testing of children and also for
cochlear implantation. The high levels of care available allow surgery on the
very young, those with multiple medical problems and those needing multi
disciplinary care. There are resident ENT registrars, but the fellow’s
operating lists do not clash with the residents.
My weekly
role at Westmead was to perform round window electrode placements under
general anaesthetic for electrophysiological assessment of cochlear function.
This involved surgery on babies down to a few months of age, which gave me
great confidence in dealing with the middle ear in such infants. I had not
previously performed such surgery on young babies. It is also a great
opportunity to talk to Prof and Dr Sanli (the SCIC Biomedical Engineer) about
the recordings and the problems of hearing assessment in the very young. Dr
Sanli has firmly held views on the best testing methodology, and I became
adept at reading the ECOG traces.
A unique
feature of this testing regime is the ability to perform electrically
stimulated auditory brainstem readings (EABR). This technique relies on a
modified cochlear implant being used to feed a test signal through the round
window electrode to stimulate an EABR. It is useful in the profoundly deaf ear
where no ECOG threshold was detected. A clear response enabled the implant
team to be very reassuring to the parents when discussing the likely outcome
of implantation. Conversely a poor result, especially in conjunction with a
poor radiological appearance to the Auditory nerve led to a very guarded
prognosis.
I felt
that for the parents of deaf children, who have many concerns and
uncertainties, the information obtained from this rigorous assessment provided
confidence in both the technology of modern cochlear implantation and in the
team that was looking after their child.
Fortnightly
Prof has a half day operating list at Westmead. Generally this is used for a
cochlear implant (CI). The list provides excellent supervised operating with
the fellow performing every case. Here I was able to progress from performing
the cortical mastoidectomy at the beginning of the fellowship to being able to
perform the whole implant procedure (without operative assistance, though
supervised) at the end of my time.
I came
across many unusual cases and in particular I will not forget a patient who
had a bifid facial nerve, with one limb passing over the stapes. This case
alone convinced me that continual facial nerve monitoring during cochlear
implantation is necessary. Other interesting cases included CSF gushers and
Mondini deformity cochleae.
The
Sydney
Cochlear Implant Centre (SCIC)
Every
Wednesday I accompanied Prof to his clinic and CI meeting at this centre. The
centre itself is housed in spacious accommodation in the grounds of the old Gladesville
Psychiatric Hospital
. As is often the case with such institutions the grounds are beautiful and
provide a very pleasant working environment.
The weekly
CI meetings are very educational. Issues relating to implantation problems in
the SCIC population are discussed. As the centre has almost 1000 patients
there are all manner of unusual problems to solve. The presence of experts in
surgery, habilitation, speech therapy and electronics (namely Dr Sanli) allows
for interesting discussions.
An
interesting aspect of work here was the constant search for charitable
funding. The programme has many streams of revenue but every opportunity to
secure funding for one extra implant is used. This attitude had enabled the
program to become the largest in Australia, and is quite inspiring.
Many of the people at the centre have personal knowledge of the wonderful results of
cochlear implantation as their children or partners are patients here as well.
The whole environment was familial and the fellow is valued.
After the
meeting I assisted Prof in the paediatric clinic, which is largely for seeing
children referred for candidacy assessment. Prof implanted the world’s first
paediatric multi channel CI recipient in 1987 and her amazing progress
catalysed the development of CI programs across the world. Consequently the
centre has an international reputation and receives many candidates from
abroad. One such case proved to be the most challenging of my fellowship time.
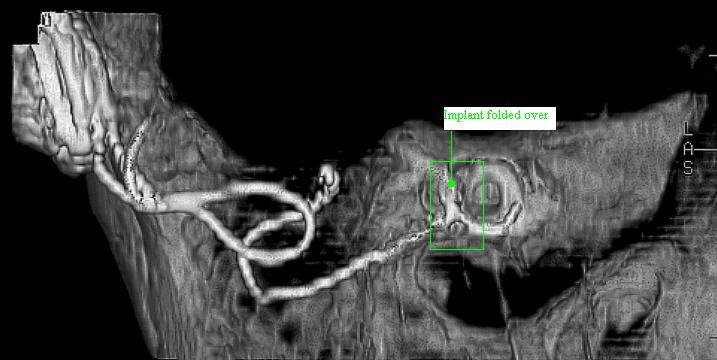
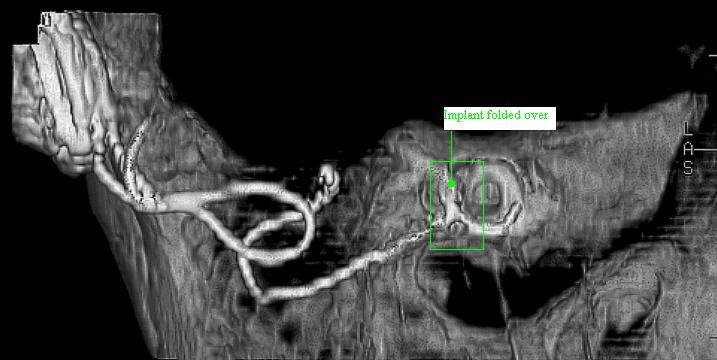
Miss X was
a fourteen year old child who had become deaf following meningitis one year
previously. She had received a CI in her home country within a few weeks of
the meningitis but had not been able to hear anything through it since it was
implanted. Dr Sanli tested the implant and felt that it was working but that
an alternative device type might be better. CT scanning showed that the other
cochlear was ossified.
Prof and I
operated on her a few weeks later. In a mammoth eight hour procedure we first
repositioned and then replaced the first device, ultimately performing a
cochlear drill out and laying a straight electrode array into the cochlea bed.
Sadly intra-operative testing did not yield promising results and as planned
we proceeded to the other ear. Here the cochlea was ossified, and on this side
Prof inserted a double array.
I was
pleased to hear that after considerable mapping and adjustment the patient is
now receiving some useful audition, albeit less than we had first hoped for.
The
Mater
Hospital
,
North Sydney
Professor
Gibson has all day operating at this private facility every other Friday and
on other days as required. These days provide excellent surgical training. We
often performed 3 CI and two other major ear cases in one list. Dr Sanli is
present for most lists and his input is invaluable.
During CI
operations Dr Sanli tests the implant before insertion, and then again after
insertion. Using an implant derived EABR he can confidently tell the surgeon
that the implant is correctly located and working. This information is relayed
to the parents and carers on the ward and provides great reassurance some time
before the patient is ready to return to the ward. Dr Sanli also provides
intra-operative testing during stapedectomy, allowing the surgeon to be
confident that a good result has been obtained.
Much of my
surgical teaching was during the Mater lists. Profs teaching technique allows
the fellow to progress according to his skill level. I never felt
under-supported but always felt that I had made technical progress at the end
of the week. This constant drive to improve helped me in many different areas.
One example was my techniques for the Bone Anchored Hearing Aid (BAHA). I had
performed this kind of surgery before but I learnt new ways around the common
problems of excess bleeding and poor wound healing that often accompanies such
operations. I felt that Prof’s teaching provided me with the best possible
surgical “finishing school”.
The Mater
hospital itself is luxurious and having been used to the décor and catering
of the NHS working in a first class private hospital also provided a welcome
insight into how pleasant the patient’s experience can be, when funding is
more plentiful.
Educational
Opportunities
In
addition to the clinical teaching already outlined I was able to benefit from
several special opportunities. The Australian Society of Head and Neck
Surgeons (ASOHNS) annual meeting was in
Sydney
this year and I was able to attend this. Professor Gibson kindly funds the
registration fees for the fellow. The conference covered many aspects of
otolaryngology and gave me the opportunity to meet many interesting people.
Amongst these were Professor Alec Salt from St Louis,
USA, who is an expert in the field of cochlear micromechanics and perilymph flow.
I was later able to hear him speak again at the New South Wales Meniere’s
Society meeting and found his theories on the pathophysiology of this
enigmatic condition fascinating.
I was also
introduced to Professor Stephen O‘Leary from Melbourne. This proved to be a fruitful meeting as I was able to spend some time with
him at the RPAH temporal bone dissection course, which I attended and assisted
at. Dr O’Leary was able to show me the Virtual temporal Bone which he has
been developing with the Commonwealth Scientific
and Industrial Research Organisation (CSIRO), and which may well prove a
useful adjunct to temporal bone dissection training for the future. The
temporal bone course had excellent speakers from around Sydney, and I learnt a great deal.
I later
visited Dr O’Leary and his colleagues in Melbourne. He kindly showed me around the hospital, laboratories and the Cochlear
Companies facilities there. I was able to spend an afternoon with Dr Robert
Briggs in the CI clinic and see a different approach to assessment of CI
candidates. During my second day in
Melbourne
I spent time in theatre with Dr Briggs and Dr O’Leary. This was most useful
as Dr Briggs is focusing his practice on hearing preservation during
implantation, and showed me some of the surgical techniques that might enable
this. The highlight of this trip though, was meeting Professor Graeme Clark at
the Bionic Ear Institute. This was a great honour for me.
I also
attended a satellite workshop at ASOHNS on facial-plastic surgery and was
invited to Cochlear’s “Breaking the Silence” symposium on cochlear
implantation in older age. This was a star studded event in the
Natural
History
Museum
. One of the most interesting speeches was from former Prime Minister Fraser.
He recounted how, as minister for industry, he received a plea for extra
funding from Professor Clarke to fund a little known technology called
the multi-channel cochlear implant. He was sufficiently impressed by
Professor Clarke’s commitment that he “took a chance” and supplied the
necessary governmental support to complete the initial development and start
the CI program. The rest, as he said “is history”.
Like some
of the previous fellows I was also able to spend a day with the Royal
Australian flying Doctors. Dr Neil Boustread, an ENT surgeon in
North Sydney
, and former fellow of Prof’s, flies out to Brewarina once every couple of
months. I was able to join him and a registrar on this three hour plane flight
into the outback. Medicine here is very different to downtown Sydney. The clinic building is well equipped but hospital facilities are distant.
For instance a CT scan is a 2 day trip for the patient and is not untaken
lightly!
One of the
most bizarre things that happened during the fellowship was that during this
flying doctors trip I met an old friend of my family’s from
Sri Lanka
. Dr Victor Benjamin has been a general practitioner in the outback for almost
20 years. He was Professor of General Surgery in Jaffna,
Sri Lanka, but left during the civil unrest. He referred the second patient I saw that
day and since I recognised his name I phoned and spoke to him. Three hours
later, as we were finishing the clinic, Dr Benjamin and his wife appeared,
having driven their 4X4 across the mud to meet me. I had not seen him since he
visited my parents in
Birmingham
some 25 years ago. My father was delighted that I should happen upon his old
friend and it struck me how small the medical world can be.
I was also
able to spend some time with the other famous Professor of Otolaryngology in
Sydney, Paul Fagan. I observed his unique techniques for dealing with canal
exostoses and also watched him skilfully deal with a difficult revision
stapedectomy. He performed this under local anaesthetic, and although it
relies on a compliant patient, does offer a level of reassurance during high
risk surgery.
Research
Projects
The
fellowship offers many opportunities for performing research projects. During
my time I pursued three projects, two of which have progressed well. The first
project was to look at the outcome of cochlear implantation in cases were
there was radiological evidence of a hypoplastic auditory nerve. Detailed
analysis of eight cases was performed, and although the outcomes were much
poorer than in children with normal anatomy, there was evidence of some
benefit. This partly contradicts the often quoted view that a hypoplastic
nerve is a contra-indication to implantation. This paper is in preparation for
submission to Cochlear Implantation International.
The second
project was to analyse the results of over 1500 ECOGs performed during the
last 7 years on patients with suspected Meniere’s disease and compare these
to controls. This data is being prepared for submission to Acta and shows the
diagnostic accuracy of tone burst testing compared to the traditional click
AP/SP ratio.
The third
project involved trying to assess whether a posteriorly placed cochlea led to
a difficult electrode insertion. Professor Gibson presented on “the
backwards twisted cochlea” at the Czech Republic for the Symposium on
Hearing Disorders in Early Childhood in Prague in May 2004, and cited me as a
co-author. It is hoped that further work on this subject may allow a full
paper to be written in the future.
Social
Events
Prof and
Alex Gibson are wonderful hosts. My family and I enjoyed several trips out on
Prof’s boat and we met again at many evening functions. One highlight was
the cochlear dinner during ASOHNS. This was held at
Fort
Dennison
on
Pinchgut
Island, which is situated in the middle of the bay and has tremendous views of the
Bridge and Opera house.
Sydney
is a fabulous city for a young family and we enjoyed our
time there more than I can describe. We were also able to travel, and saw the
Great Barrier Reef
and the
Blue Mountains
. We sampled wine in
Hunter
Valley
and went whale watching off
Fraser
Island. Our memories and photos have now bored our families, but remain very dear to
us.
Career
Benefits
I hoped
and expected that undertaking this fellowship would make me more attractive to
future employers but this belief was confirmed early in the year. A
consultants post, with a special interest in Otology at St Georges Hospital
was advertised in February. I returned from Sydney
for the interview for this post and I was successful in obtaining it. During
the interview it was quite clear that my further training in otology was of
great interest and I am sure that it helped me secure the post.
Summary
I hope I
have expressed the tremendous admiration I have for this fellowship. The
training experience is unique, the city and country breathtaking and Professor
Gibson is inspiring in so many ways. I feel greatly privileged to have been
one of the Graham Fraser Memorial Fellows and my family and I are very
grateful for the opportunities the fellowship has afforded us.